Reheating a Cold Case
In criminal investigation, it is well known that passing time obscures the facts, making what happened more difficult to discern. Eventually, the case turns cold - unlikely to be solved unless we discover new evidence. In some ways for over a century, epidemiologists have been dealing with just such a cold case, picking through the rubble of the 1918 Influenza pandemic and trying to make sense of what they find. But as we will see, debate continues in a number of areas.
Researchers have argued whether 1918's influenza was somehow implicated in the 1915 to 1926 epidemic of the neurological disease encephalitis lethargica, and pondered the link with a following spike in Parkinson's disease. It would be premature to state that such issues are fully settled, with adherants to various theories still arguing their corner. Another debate surrounds the idea that the 1918 pandemic effects reached deep into the second half of the twentieth century, by reducing future attainment for babies in the womb. Perhaps most controversial of all is the theory that 1918 drove a huge wave of cardiovascular disease peaking more than four decades later.
Much as we'd prefer it to be otherwise, many questions like those raised above are unlikely to be definitively settled. Had researchers been on the scene at the time, with access to survivors and today's medical technology, some of these debates would have become robust findings. Detectives have the concept of the Golden Hour for gathering information after a crime, and what works for criminology doubtless stands for epidemiology as well. However, while 1918 is long gone, we may currently be in a Golden Hour for understanding the consequences of the COVID-19 pandemic. Specifically, can a viral pandemic unleash a major wave cardiovascular illness? And might there be follow-on neurological consequences?
A study of US Veterans data was recently published in Nature. It compared the health records of 153,760 COVID-19 survivors with pools of historic and current controls (both in excess of 5.5 million individuals) in order to estimate the cardiovascular impacts of the infection. US veterans are a specific population that are around 90% male and 70% white, however the modelling was adjusted to maximise relevancy for other groups too. The research found increased 12-month burdens across all classes of cardiac event amongst survivors of COVID-19 infection. This is shown in Figure 1.
Figure 1.Excess 12-month cardiac cases (per 1000) by COVID-19 infection type. Data Source: Xie, Y., Xu, E., Bowe, B. et al. 2022.
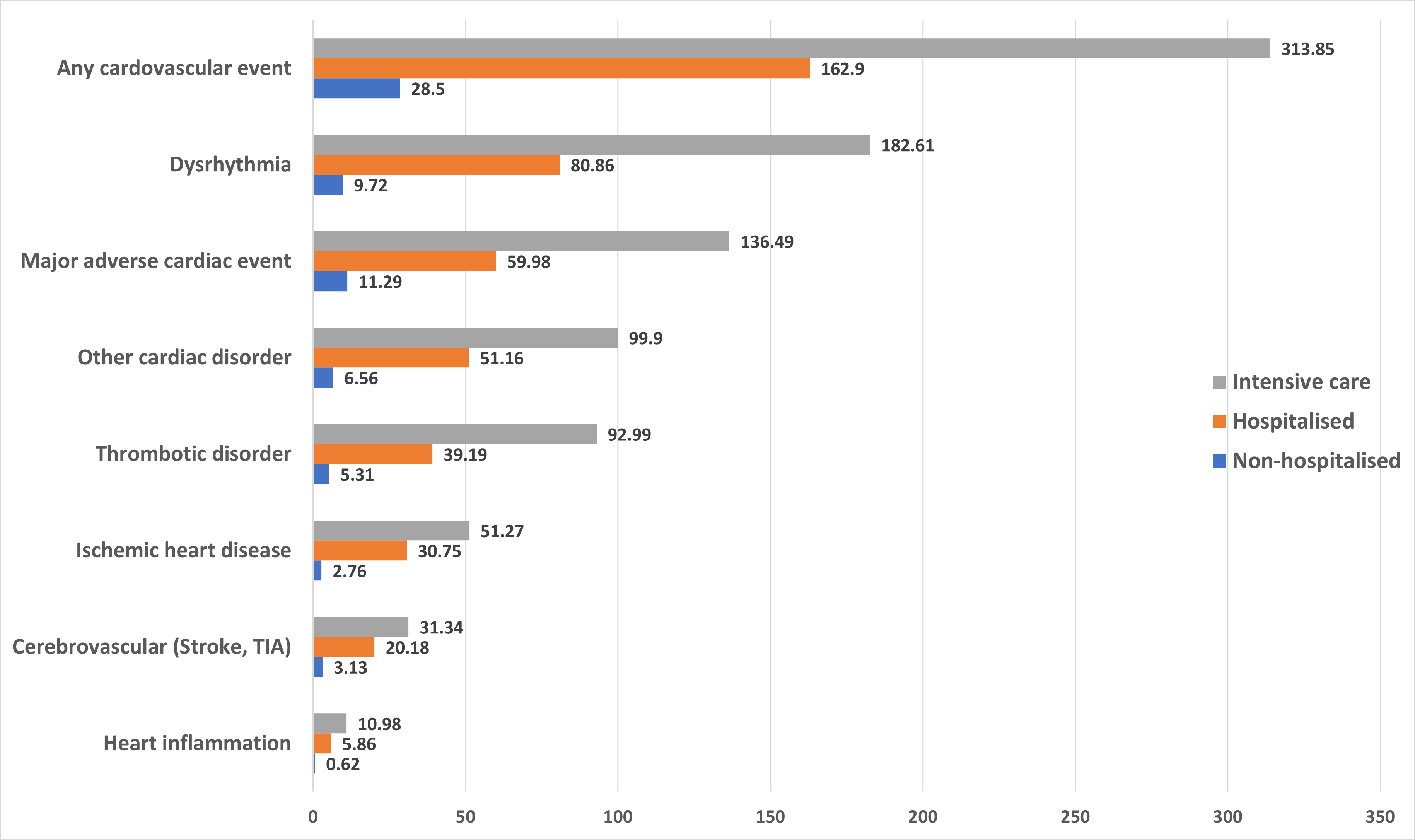
Note that the Veterans study underscores other research suggesting that COVID-19 infection constitutes a greater risk of the cardiac inflammatory conditions (myocarditis and pericarditis) that could rarely follow mRNA vaccination. Taken overall, the findings are stark - even the non-hospitalised sufferers of a so-called mild infection were found to be carrying excess cardiac risk in every category. Such excess cardiac disease risk playing out over the years following the pandemic might not look too dissimilar to the theorised cardiovascular impacts from the 1918 influenza, except here we may have the timely analysis needed to see it coming. Not stopping there, however, in research published in the BMJ, the US Veterans data was analysed once more, this time looking for neuropsychiatric impacts in COVID-19 survivors. These are summarised in Figure 2.
Figure 2.Excess 12-month neuropsychiatric cases (per 1000) by COVID-19 infection type. Data Source: Xie, Y., Xu, E., Al-Aly, Z. et al. 2022.
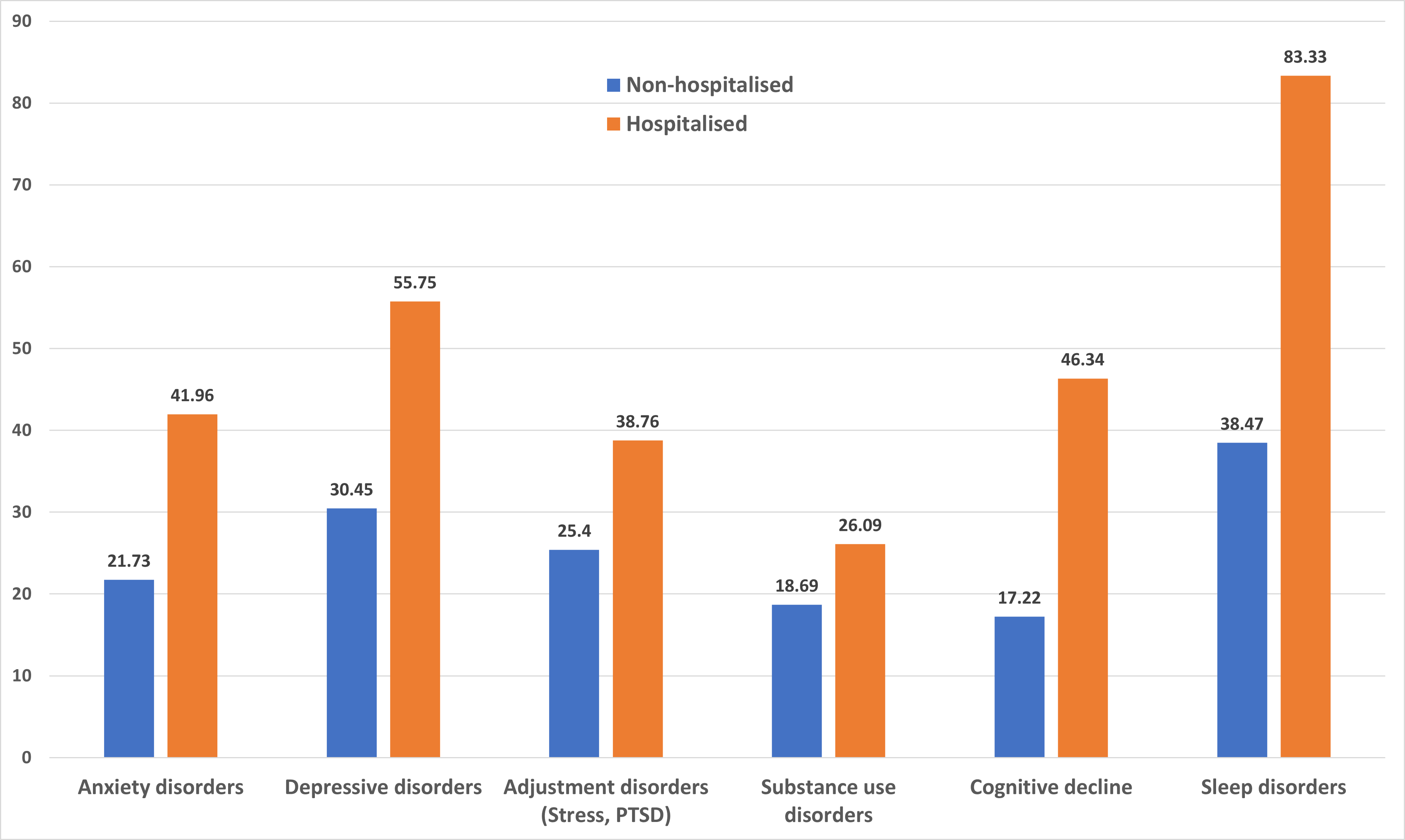
Although this study did not consider the specific (and more purely neurological) disorders spiking after 1918, we clearly see that our recent pandemic reached into the brain and increased disease burden in all categories examined. Since an excess was also evident when comparing with a historic cohort diagnosed with standard seasonal influenza, we find another strike against those who sought to minimise COVID-19 as just 'a little flu'. In short, COVID-19 continues to prove exceptional in all the wrong ways.
Since there has been much discussion of differences between SARS-COV2 viral variants, it is worth pointing out that neither of these COVID-19 studies considered the infective variant. Similarly, neither explored the protective effect of vaccination, although research from the UK COVID Symptom Study did point to an approximate 50% reduction in risk of post-infection sequelae after two vaccine doses, so vaccination seems likely to mitigate risks in the categories we have considered here. We can perhaps take additional consolation that by establishing facts during our pandemic we won't need to argue them in a century's time. And we can further hope this knowledge might reduce the future influence of public-health naysayers, seeking to deny a role for society-wide measures in protecting us against both disability and death.
References:
Xie, Y., Xu, E., Bowe, B. et al. (2022) Long-term cardiovascular outcomes of COVID-19, Nat Med (2022) doi: 10.1038/s41591-022-01689-3
Xie, Y., Xu, E., Al-Aly, Z. et al. (2022) Risks of mental health outcomes in people with covid-19: cohort study, BMJ 2022;376:e068993 doi: https://doi.org/10.1136/bmj-2021-068993
Jang, H., Boltz, D.A., Webster, R.G., Smeyne, R.J. (2009) Viral Parkinsonism, Biochim Biophys Acta. 2009 Jul; 1792(7): 714-721. doi: 10.1016/j.bbadis.2008.08.001
Almond, D. (2006) Is the 1918 Influenza Pandemic Over? Long-Term Effects of In Utero Influenza Exposure in the Post-1940 U.S. Population, Journal of Political Economy Volume 114, Number 4 doi: https://doi.org/10.1086/507154


Add new comment