'E' is for evidence
Our battle with COVID-19 has raised many questions around the evidence base for proposed public health interventions. Outside the furnace of a pandemic, such conversations might progress at a measured pace, one research paper at a time. But with infections rising and lives at stake, debates in the science community become both more heated and more public. We've seen arguments play out in news media and press conferences, debating face masks, psychological impacts of lockdown, hygiene measures and herd immunity. Now, some argue a potentially critical role for vitamin D, a debate that reached the UK parliament in the middle of January 2021.
Vitamin D is naturally created in our skin in response to sunlight, and winter in the Northern hemisphere brings a greater risk of deficiency. We know vitamin D deficiency is bad for bone-health, but some studies suggest deficiency also correlates with worse outcomes in COVID-19. Of course, human research perennially throws up contradictory studies, making it tricky to know where to stand. Regulators don't have the luxury of neutrality, so around the middle of last year UK health bodies deemed available evidence insufficient to raise recommended supplementation levels. Opponents claim currently recommended levels are inadequate for protection against severe respiratory disease.
Whether vitamin D supplementation combats respiratory infection is subject to debate, with evidence piling up both for and against. But since such supplementation is both low cost and relatively low risk, the possibility remains compelling. The first wave of infections showed that COVID-19 has a disproportionate impact on BAME populations, whom previous research has found more prone to vitamin D deficiency. In addition, obesity, another COVID-19 risk factor, is correlated with vitamin D deficiency. And most obviously, the frail elderly with the highest COVID-19 mortality rates are those least likely to spend time outdoors in the sun. Could vitamin D deficiency, something easily fixable in most people, lead to the increased COVID-19 vulnerability found in some of our communities?
Oddly enough, it was Spain that propelled the vitamin D discussion into the UK parliament. A hospital pilot study conducted in Córdoba suggested fast-acting calcifediol supplementation significantly reduced admissions to ICU. This was a relatively small study, nevertheless in November 2020 the regional government in Andalusia decided to begin supplementation in care homes. The question now is whether treating this vulnerable population may have driven a reducing mortality trend against the rising winter mortality we have seen in the UK. We explore this in Figure 1.
Figure 1. Scaled 7-day average mortality between Andelusia and Scotland. Source: own calculations using data from here and here.
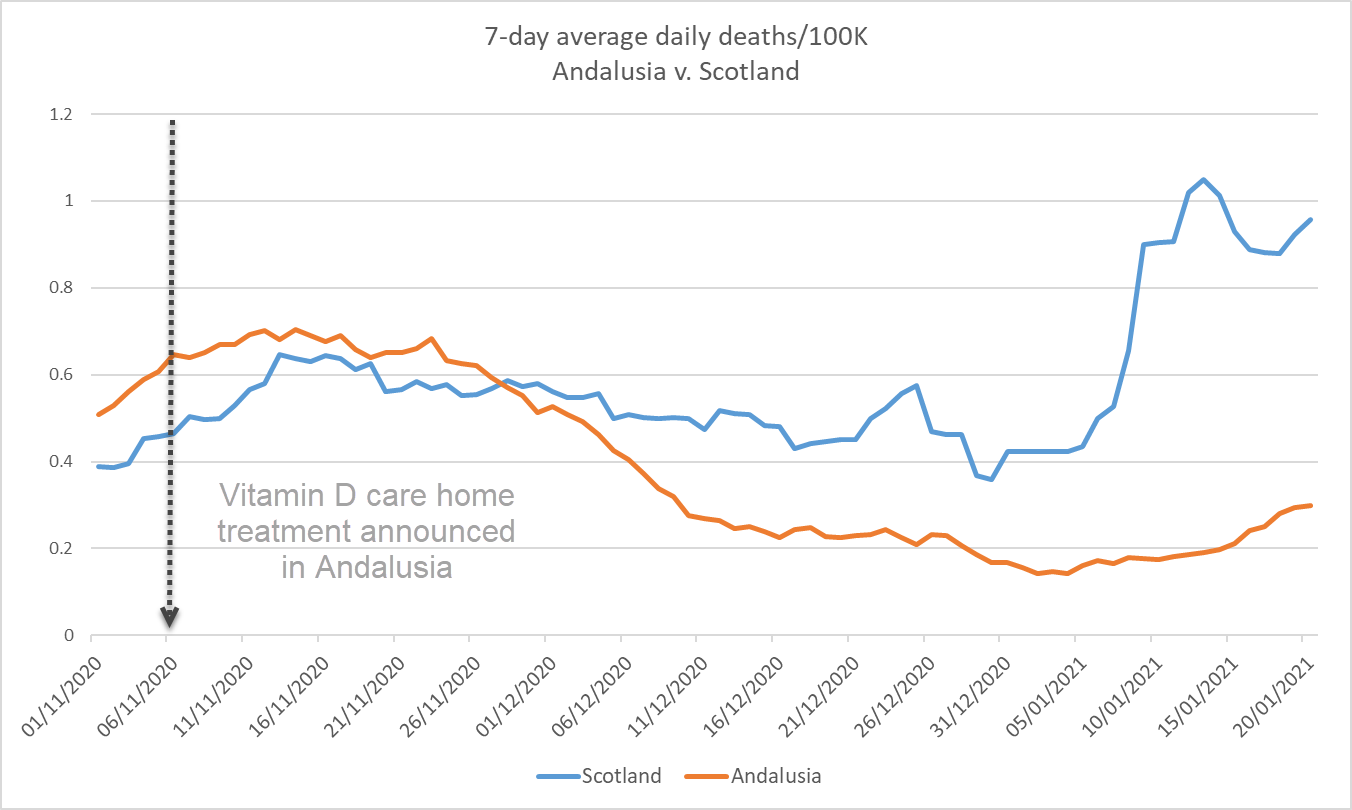
Figure 1 shows a stark difference in experienced mortality between the two territories. In Scotland the trajectory in this November-January period is clearly upwards, whereas mortality is falling over that period in Andelusia. If November's care home vitamin D supplementation was all that differed between these populations we'd likely be looking at a very exciting effect. However, we are considering two populations with different age gradients, different lockdown restrictions, and notably, Scotland is measuring large numbers of infections with the more contagious B.1.1.7 COVID-19 strain. We also see a large spike in Scottish deaths that may well indicate the impact of mixing behaviour over the festive season. For these reasons, we'll now consider Figure 2, which compares Andelusia with Spain as a whole.
Figure 2. Scaled 7-day average mortality between Andelusia and all of Spain. Source: own calculations using data from here and here.
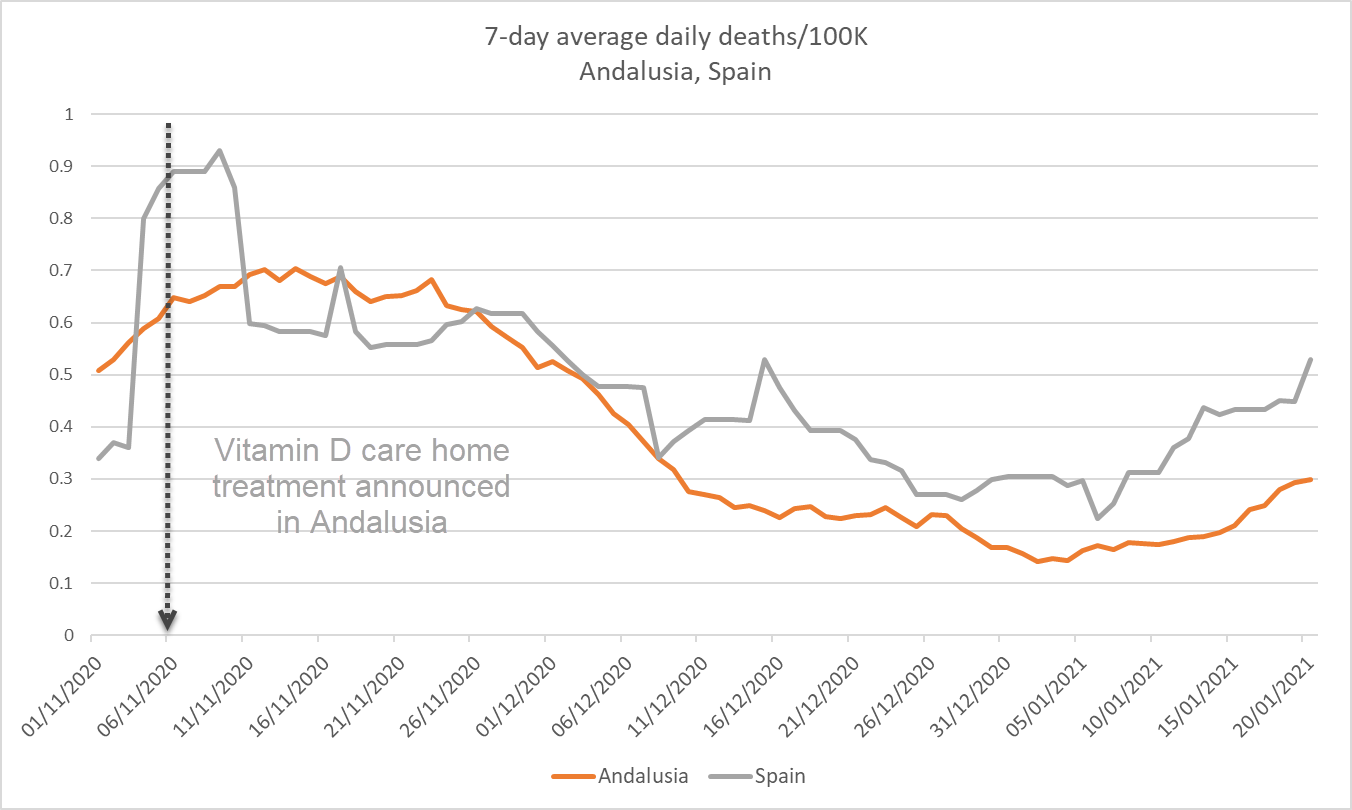
In Figure 2 the trend over that period appears to be falling in both territories, albeit perhaps more convincingly in Andelusia. The data does appear to show a divergence in trend, plausibly rooted in a November intervention, but we can't (from this data alone) attribute that divergence to a specific cause. The UK is running a further vitamin D COVID-19 study to try and answer this question once and for all.
References:
Entrenas Costa L.M. et al (2020). Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study. The Journal of Steroid Biochemistry and Molecular Biology. https://doi.org/10.1016/j.jsbmb.2020.105751
Previous posts
A Model for Reporting Delays
In his recent blog Stephen described some empirical evidence in support of his practice of discarding the most recent six months' data, to reduce the effect of delays in reporting deaths. This blog demonstrates that the practice can also be justified theoretically in the survival modelling framework, although the choice of six months as the cut-off remains an empirical matter.
Reporting delays
When performing a mortality analysis, it is my practice to disregard the most recent six months or so of experience data. The reason is delays in the reporting and recording of deaths, i.e. occurred-but-not-reported (OBNR) to use the terminology of Lawless (1994). We use the term OBNR, rather than the more familiar term IBNR (incurred-but-not-reported); IBNR is associated with "cost-orientated" delay distributions of insurance claims (Jewell, 1989), whereas we are focused on just the delay itself.


Add new comment